Revised 11/1/2007
Chapter 5: Contents Summary Introduction Cases Interpretation Repeatability Chapter 6The patient is a 30 year old Hispanic woman who is a never-smoker and who is complaining of one year of progressive episodic dyspnea with cough and wheezing. She has a history of seasonal allergies. Her chest radiograph is completely normal. Spirometry results and figures (Figure 5-1) showing the volume-time and flow-volume curves before and after the use of a bronchodilator are shown below.
Baseline - Before Bronchodilator
Age: 30 Height: 5 ft 4 in Weight: 160 lbs
| Actual | Pred | % Pred | LLN | |
| FEV1, Liters | 2.51 | 3.23 | 78% | 2.57 |
| FVC, Liters | 3.46 | 3.75 | 92% | 3.11 |
| FEV1/FVC, % | 73% | 84% | 74% |
| Actual | % Pred | % Change | |
| FEV1, Liters | 3.33 | 104% | +33% |
| FVC, Liters | 4.05 | 108% | +17% |
| FEV1/FVC, % | 82% |
Figure 5-1. Baseline (Blue) and Post (Red) Bronchodilator Spirometry
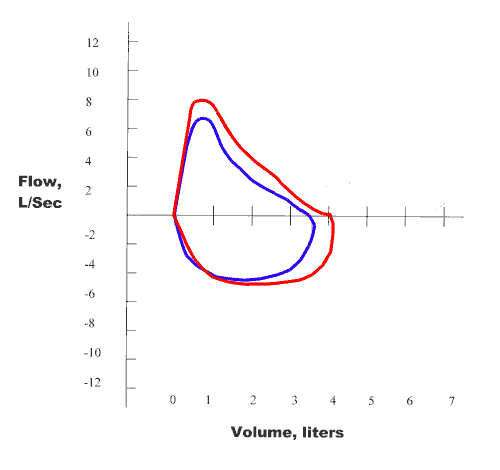
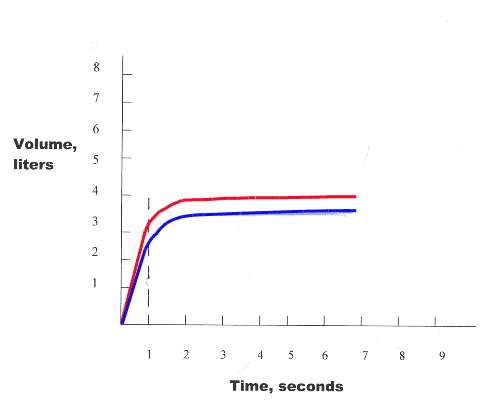
First, examine the FEV1/FVC% when compared to the LLN. Since the actual FEV1/FVC% is < LLN (73% < 74%), there is an obstructive lung defect present. Next, examine the FEV1 as % of predicted for severity of obstructive impairment. Since the value of FEV1 % of predicted is > 60% of predicted but < LLN (78% of predicted), the degree of obstruction is "mild". Then, examine the FVC to determine if it is < LLN which would suggest restriction. Since the FVC is > LLN, there is no indication of a restrictive lung defect. The patient then had a treatment with a bronchodilator with repeat spirometry to determine if there was any bronchodilator responsiveness. The value of FEV1 has increased by 33% and 820 ml. Thus, there is a significant response to the use of a bronchodilator (at least 12% increase in FEV1 with at least 200 ml increase in FEV1). Therefore, the interpretation of spirometry results for this patient is "mild obstruction with a significant response to the use of a bronchodilator".
Clinical Correlation: It appears likely that this patient may have Work-Related Asthma (Baker's asthma). She has obstruction at baseline and demonstrates a significant response to the use of a bronchodilator - results consistent with a diagnosis of asthma. Also, she could have blood tests to determine if she has specific IgE serum levels to any of the following that are associated with Baker's asthma: fungal α-amylase, barley, wheat, rye, soybean, Alternaria tenius, and Aspergillus fumigatus. Because she has obstruction at baseline, she would not be a candidate for a broncho-provocation test. However, it might be helpful to perform peak flow measurements at, and away from work, to determine if there is a pattern of work-relatedness.