Revised 11/1/2007
Chapter 5: Contents Summary Introduction Cases Interpretation Repeatability Chapter 6The patient is a 62 year old Caucasian male who is a smoker of 1 ppd for over 35 years and who worked as a pipefitter but quit 5 years ago. He is complaining of 2-3 years of progressive dyspnea with worsening cough and some phlegm production. As a pipefitter, he has had significant exposure to asbestos insulation beginning 35 years ago and lasting for 10-15 years. His chest radiograph reveals diffuse interstitial markings of irregular small opacities especially in the lower lung fields with some pleural abnormalities (see Radiograph). (note: heart surgery with sternal wires)
Age: 62 Height 5 ft 11 in Weight 212 lbs. Baseline Results
| Actual | Pred | % Pred | LLN | |
| FEV1, Liters | 1.96 | 3.67 | 53% | 2.86 |
| FVC, Liters | 3.18 | 4.86 | 65% | 3.92 |
| FEV1/FVC, % | 62% | 75% | 66% |
| Actual | % Pred | % Change | |
| FEV1, Liters | 2.00 | 54% | +2% |
| FVC, Liters | 3.22 | 668% | +1% |
| FEV1/FVC, % | 62% |
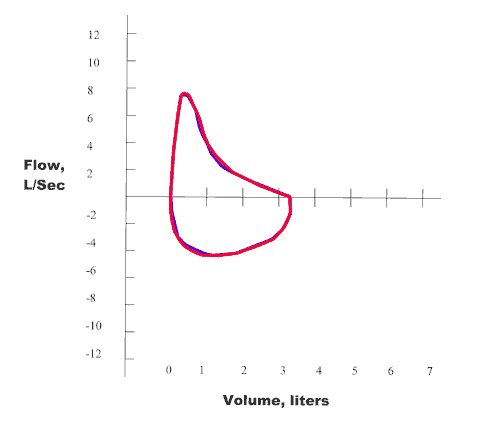
Figure 5-2. Spirometry - Baseline (Blue)
and Post Bronchodilator (Red).
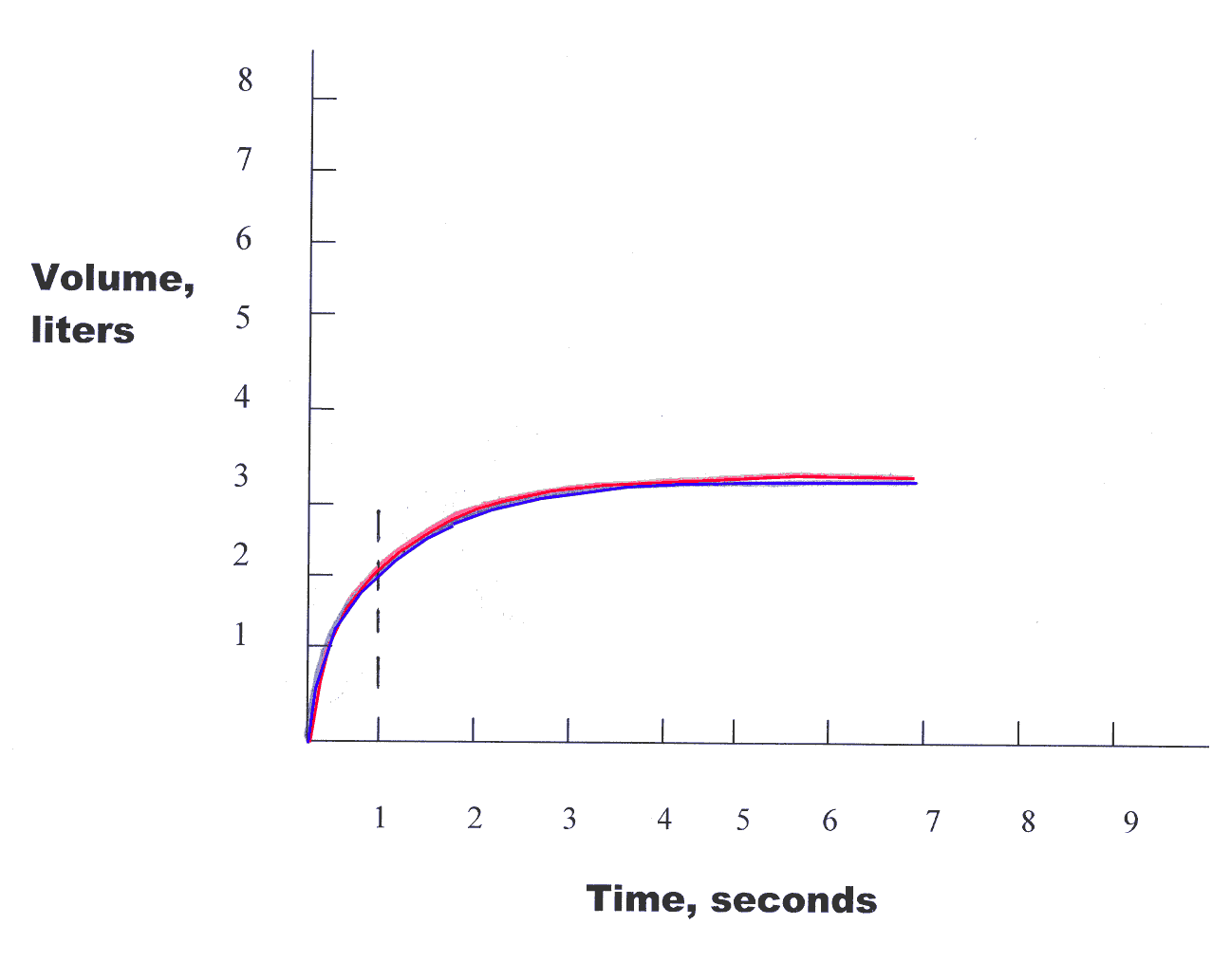
First, examine the FEV1/FVC%
when compared to the LLN. Since the actual
FEV1/FVC% is < LLN (62% <
66%) there is an obstructive lung defect present.
Next, examine the FEV1
as % of predicted for severity of obstructive impairment. Since the value of
FEV1 % of predicted is between 41-59% of predicted (53% of predicted), then the
degree of obstruction is "moderate".
Next, examine the FVC to determine if it
is < LLN which would suggest restriction. Since the FVC is < LLN
(3.18 < 3.92),
there is indication of a restrictive lung defect. The severity of restriction is
determined by the % of predicted for the FVC. Since the
FVC % of predicted is
> 60% of predicted but < LLN, then the degree of restriction is "mild".
The patient then had a treatment with a bronchodilator
with repeat spirometry to detemine if there was any bronchodilator
responsiveness. The value of FEV1
has increased by only 2% and only 40 ml.
Thus, there is no significant response to
the use of a bronchodilator (at least a 12% increase in FEV1
with at least a 200 ml increase in FEV1).
Therefore, the interpretation of spirometry for this patient is a "mixed pattern
with moderate obstruction as well as mild restriction with no significant
response to the use of a bronchodilator."
Clinical Correlation: It appears that this patient has asbestosis with other radiographic findings that would be consistent with asbestos exposure (pleural abnormalities). Further confirmation of this diagnosis could include complete lung function tests with lung volumes to confirm restriction and diffusing capacity measurement to determine if there is a decrease in this value as might be expected with asbestosis. Given the patient's smoking history, there may also be a component of Chronic Obstructive Pulmonary Disease (COPD). To complete the evaluation, either a B-Reading of the Chest Radiograph or preferably a CT scan of the chest to document the radiographic findings and see if there may be accompanying emphysematous changes from his smoking history.