Revised 11/1/2007
Chapter 5: Contents Summary Introduction Cases Interpretation Repeatability Chapter 6The patient is a 41 year old African-American woman who is a bus driver, never-smoker who has complained of 1-2 year history of progressive dyspnea and daytime sleepiness with snoring at night. She has fallen asleep on her job as a bus driver. Her chest radiograph was interpreted as low lung volumes but no infiltrates.
Age: 41 Height 5 ft 8 in Weight 348 lbs
| Actual | Pred | % Pred | LLN | |
| FEV1, Liters | 1.48 | 2.89 | 51% | 2.20 |
| FVC, Liters | 1.72 | 3.53 | 49% | 2.73 |
| FEV1/FVC% | 86% | 82% | 71% |
| Actual | % Pred | % Change | |
| FEV1, Liters | 1.50 | 52% | +1% |
| FVC, Liters | 1.72 | 49% | +0% |
| FEV1/FVC% | 87% |
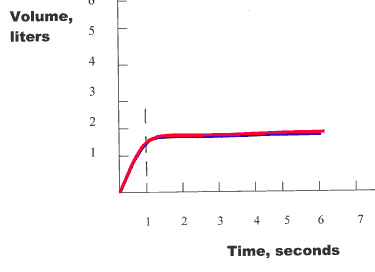
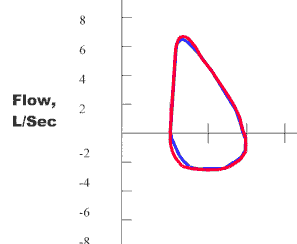
First, examine the FEV1/FVC%
when compared to the LLN. Since the actual
FEV1/FVC% is > LLN (86% >
73%), there is no obstructive lung defect present.
Next, examine the FVC to
determine if it is < LLN which would suggest restriction. Since the
FVC is < LLN,
there is indication of a restrictive lung defect. The severity of
restriction is determined by the % of predicted for the FVC. Since the
FVC % of
predicted is < 50% of predicted (49% of predicted), the degree of
restriction is "severe".
The patient then had a treatment with a bronchodilator
with repeat spirometry to determine if there was any bronchodilator
responsiveness. The value of the FEV1
has increased by only 1% and only 20 ml.
Thus, there is no significant response to
the use of a bronchodilator (at least a 12% increase in FEV1
with at least 200 ml increase in FEV1). Therefore, the interpretation of
spirometry for this patient is "severe restriction."
Clinical Correlation: It appears that this patient may have obesity related restrictive lung disease as well as possible significant obstructive sleep apnea (OSA). More complete evaluation would include complete pulmonary function studies including lung volumes to confirm the presence of restriction and diffusing capacity which should be fairly maintained. In addition, arterial blood gases may be useful to determine if she has a component of obesity hypoventilation syndrome with elevation in pCO2. Finally, an overnight polysomnography study is indicated for documentation of the presence and severity of Obstructive Sleep Apnea with determination of the appropriate settings for CPAP or BiPAP to be used at night for treatment.